Diagnosing Pain
Another stellar blog post with fresh perspectives on healthcare from our PA, Craig Kantack. Craig has been with Eastern Idaho Spine, Sports and Rehab for over 3 years and is really an expert in PHYSIATRY and musculoskeletal care. ----- 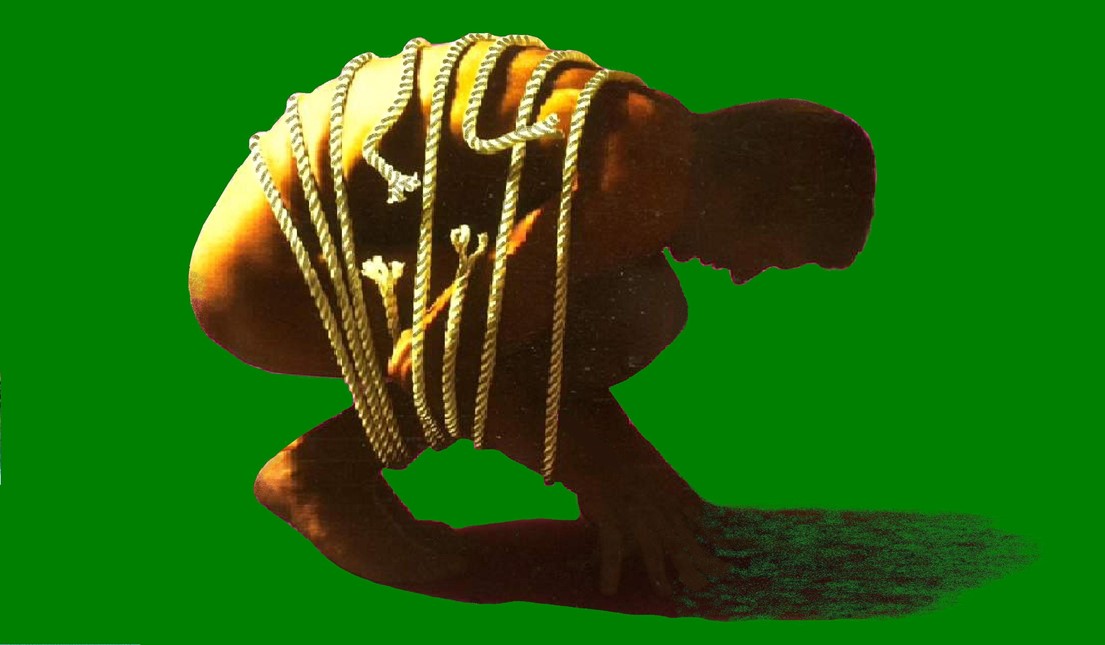 As a PA walking into the exam room for the first time (new patient) or for that matter any other appointment, I diligently try to keep an open mind. By this, I mean trying to avoid the pitfalls we in the medical world call anchoring. Anchoring is where one determines the diagnosis prior to seeing the patient or after seeing the patient for several visits, assuming it will be the same result each time. This is often why I take a quick look at the imaging before entering the room and then a much more thorough review after I have all the facts.
As a PA walking into the exam room for the first time (new patient) or for that matter any other appointment, I diligently try to keep an open mind. By this, I mean trying to avoid the pitfalls we in the medical world call anchoring. Anchoring is where one determines the diagnosis prior to seeing the patient or after seeing the patient for several visits, assuming it will be the same result each time. This is often why I take a quick look at the imaging before entering the room and then a much more thorough review after I have all the facts.
Nobody is perfect, however, and everyone has been guilty, at times, of following the path of the obvious. My plan for this blog was to give a brief/condensed explanation of diagnosing pain. Determining the cause of a patient's musculoskeletal pain can be truly challenging. Pain is subjective, you cannot see it or objectively test for it---it is a person’s response to a condition. Perceptions vary greatly as 2 people with the same condition will have 2 different responses. Contrast this with an objective finding such as a laceration or fracture---those conditions you can see/feel---they’re obvious. In Physiatry, we cover a wide array of symptoms and conditions. As a previous mentor put it, “The pool is wide and deep.” So, with the introduction completed we can move forward. When a patient comes to our clinic it is often due to pain---this is logical as seldom is the chief complaint, “Craig, I can’t throw a baseball as fast, or I can’t run as far.” But rather, “I’m having this intense pain that is affecting my sleep and work, I can’t live like this.” Therefore, what is pain? Pain comes in 2 flavors, nociceptive and neuropathic.
- Nociceptive is pain that arises from the musculoskeletal system. This type of pain can be broken down to somatic and visceral. Somatic pain is from the musculoskeletal system skin, bones, muscle, connective tissue and joints. Visceral pain arises from the organs of the body.
- Neuropathic is pain that arises from trauma/damage and association with the nervous system: examples include RSD, Fibromyalgia and Shingles.
Back to walking into the room, when I enter my role is to determine what the true pain generator is, what is causing the patient’s discomfort and the best way to treat it. Once this is decided, we develop a plan and move forward. On paper, it sounds quite simple, but in reality it can be very complicated and tricky based on the presentation and history. For example, let's take two patients have low back pain: The first has no prior history and on MRI has one disc protrusion, while the other has an extensive history including surgery and multi-level issues on imaging. In theory, the second patient is going to be more challenging to narrow in on exactly what is causing their pain. However, one needs to be careful on the first patient to confirm the disc bulge is indeed the problem and not anchor on it. Once a direction is decided, we have several tools at our disposal.
My goal is to formulate the most effective/efficient and least invasive plan using any and/or all the tools available. Due to its subjective nature, not always does one hit a home run the first time up to bat---at times it can be a process as we use a patient's responses/feedback to tune in on the true pain generator. Always know that we do our best to treat you the patient, you are not a number, you are a person that we care about and to use a bad pun, “we got your back.” (we treat a lot of patients with back pain!) Keep moving! Craig and all the staff at EISSR
